Canadian scientists find new way to attack antibiotic-resistant lung infections
Enzymes used to break down the walls built by microbes
Canadian scientists have discovered a possible way to break through the defences of some antibiotic-resistant respiratory infections. It’s hoped that the findings could someday benefit people with cystic fibrosis and other chronic lung diseases who are at greater risk of infections.
 The research looked at biofilms, which are one of the main causes of hospital-acquired infections. Microbes form biofilms on surfaces like the insides of our lungs, heart valves and artificial hips. In fact, implanted medical devices could account for up to 70 per cent of hospital-related infections, according to previous research.
The research looked at biofilms, which are one of the main causes of hospital-acquired infections. Microbes form biofilms on surfaces like the insides of our lungs, heart valves and artificial hips. In fact, implanted medical devices could account for up to 70 per cent of hospital-related infections, according to previous research.
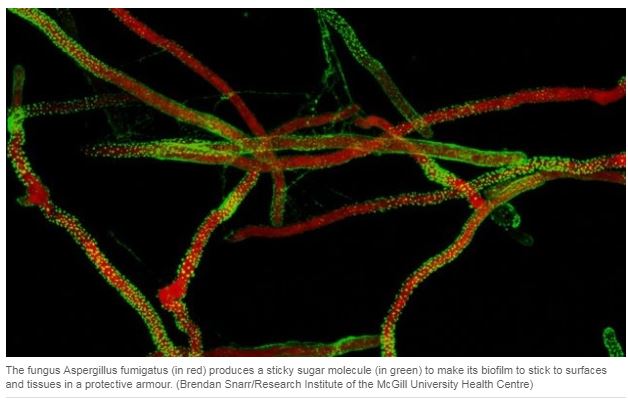
For doctors and scientists, biofilms have been a tough nut to crack. That’s because some bacteria and fungi secrete a matrix of sugar molecules to form the biofilm armour — a physical and chemical barrier to keep antibiotics and our immune cells out so they don’t have a chance to kill the pathogens.
Think of how humans shifted from life as hunter gatherers to building up walls around their town to protect themselves from invaders, said Sheppard, a clinician-scientist at the Research Institute at McGill University Health Centre in Montreal. Some bacteria and fungi build a biofilm matrix, a type of city wall to defend their communities.
Sheppard and Howell were the lead authors of a study published in the journal of the Proceedings of the National Academy of Sciences in June. They focused on two microbes that are responsible for lung infections: Aspergillus fungi and Pseudomonas aeruginosa bacteria.
In test tube experiments, the researchers discovered that the microbes use enzyme “saws” to cut and then build the walls of their biofilm homes out of uniform pieces, like two-by-four pieces of lumber.
They were able to turn the microbe’s defence against itself, using its machinery to engineer the enzymes and control where the cuts were made. Instead of small, uniform wooden boards, the biofilms were cut into the equivalent of 10-foot-long pieces. The microbes weren’t able to use those unwieldy pieces to repair the gaping holes scientists inflicted on the biofilm walls.
“We made the uncontrolled versions, which cut willy-nilly and destroy the biofilm,” Sheppard said. “Lo and behold the enzymes worked in an animal model,” Sheppard said. Specifically, it was a lung infection model of Aspergillus fungus in mice.
It took 10 years of basic laboratory research to prove it was the enzymes at work. They also discovered that both the fungi and bacteria used the same tool, which was active across the two species.
Howell, a senior scientist at SickKids and a professor of molecular biology at the University of Toronto, said when they realized they understood the mechanics well enough to apply the approach more broadly, “it was like one of those light bulb moments” in science.
The discovery could be applied therapeutically, said Howell, in the form of biofilm-busting enzyme therapy for people with cystic fibrosis and other chronic lung diseases. In the case of CF lungs, Howell said the underlining genetic defect prevents cilia, or small hairs on the surface of the airway, from doing their job of beating together to move mucus up and out of the lung.
The airways in people with CF also provide an ideal environment for some bacterial infections to take hold.
Whether the engineered enzymes work the same in humans as in mice, without toxic effects, remains to be seen. Sheppard estimates the first studies in people are at least five years away.
